This article is an excerpt from the Shortform book guide to "Being Mortal" by Atul Gawande. Shortform has the world's best summaries and analyses of books you should be reading.
Like this article? Sign up for a free trial here.
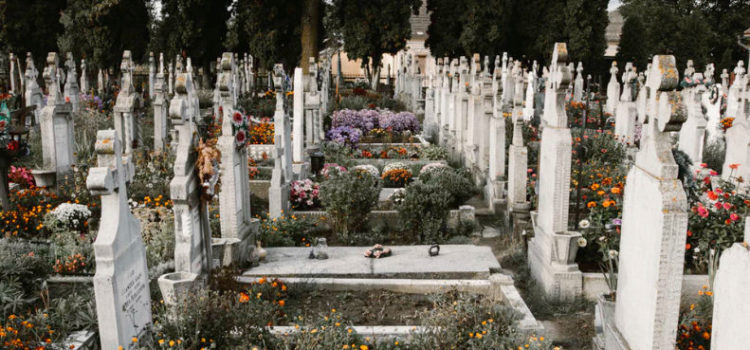
What matters most at the end of life? How can end-of-life institutions help their patients prepare to die with dignity and peace?
The dying should have the chance to wrap up their affairs, share their deepest thoughts, encourage their loved ones, and establish their legacies. However, modern-day end-of-life institutions tend to deprive their patients of the opportunity to decide how they want to spend their final days.
Here’s why we should make our end-of-life decisions before they are made for us.
End-of-Life Healthcare
According to Gawande, we can significantly improve our approach to dying by being judicious in our end-of-life healthcare. This involves being decisive about what we want and resisting the urge to address every ailment the dying face.
In his book Being Mortal, Gawande insists we should decide exactly what we want for our last days. Do we want to undergo every possible life-saving treatment? Or are we willing to forego treatment so we can stay clearheaded and have more time with our loved ones? Should doctors try to resuscitate us? Or will we let our bodies naturally give out? We must consider these difficult questions if we hope to give ourselves and our loved ones peace and closure in our final moments.
(Shortform note: Gawande doesn’t specify when we should plan our end-of-life care, just that we should plan it. We have to be in a sound state of mind to plan it, so we should do it while we’re still capable of expressing our wishes and making complicated decisions. This planning typically involves several components, such as creating a living will (also known as an advanced directive), securing life insurance, determining what lifesaving measures you’re willing to receive (such as CPR or intravenous fluids), where you’d like to receive your end-of-life care, how you want your body to be handled after death, and so on. The process can be stressful and demanding, so make your end-of-life decisions before they become urgent.)
If we don’t decide how we want to live our final days, we’ll likely get caught up in the inertia of our modern, medicalized approach to dying, which will undermine our ability to find peace. The dying are often barraged with endless treatments and relegated to the isolation of a hospital ward, unable to experience closure as they should.
(Shortform note: Some experts disagree with Gawande’s perspective, arguing that hospitals provide a level of care and expertise that’s critical for dying patients and their loved ones. Beyond providing around-the-clock access to advanced medical technology, hospitals can provide social support and a better avenue to closure for the bereaved. When a loved one dies at home, painful memories become associated with that place, but when a loved one dies in a hospital, the memory of the death is separate from the home. Despite such advantages, these experts argue that hospitals must work to maintain privacy for patients, preserve their dignity, and respect their wishes about end-of-life care.)
Hospice as a Model for Judicious End-of-Life Care
According to Gawande, hospice contrasts with this approach and is a model of judicious end-of-life healthcare. It’s designed to support the well-being of the dying and their loved ones by helping them determine and focus on their urgent end-of-life priorities. It reduces or eliminates invasive treatments in favor of comfort and peace. Hospice caretakers reduce distractions for their patients so they can find closure: They treat the process of dying as a natural experience patients can meet with clarity and calm.
Gawande writes that this form of care has been shown to extend the lives of patients when compared with traditional interventionist medical care, but it’s not practiced as widely as it should be. More should be done, he suggests, to make hospice care commonplace.
(Shortform note: Despite the benefits of hospice care, the World Health Organization recently estimated that only 10% of people in the world who need such care receive it. Most of those who don’t receive this type of care live in low- and middle-income countries. In the US, the Medicare hospice benefit (enacted in 1983) has made access to hospice generally affordable, yet the care is used by only half of the eligible population. Hospice professionals note that many are simply unaware of how to access the care they need. They suggest that you should discuss hospice options with your healthcare provider whether you or a loved one is presently in need of the services or not.)
———End of Preview———
Like what you just read? Read the rest of the world's best book summary and analysis of Atul Gawande's "Being Mortal" at Shortform.
Here's what you'll find in our full Being Mortal summary:
- What it's like to age and die in the 21st century
- Why we need to be better at accepting death
- How to improve the well-being of the aging and dying






